Phase 2: COVID-19 Directives for Eeyou Istchee
Quick Navigation
Quickly Access COVID-19 Directives for Eeyou Istchee
Click on the link to navigate the page
About Phase 2 - June 22, 2020
The last case for Eeyou Istchee was May 1st, 2020 demonstrating that the commitment of the leadership and people of Eeyou Istchee to the current approach is sound.
Therefore, Phase 2 can proceed in accordance with the following measures and restrictions:
- Increasing the size of outdoor social gatherings
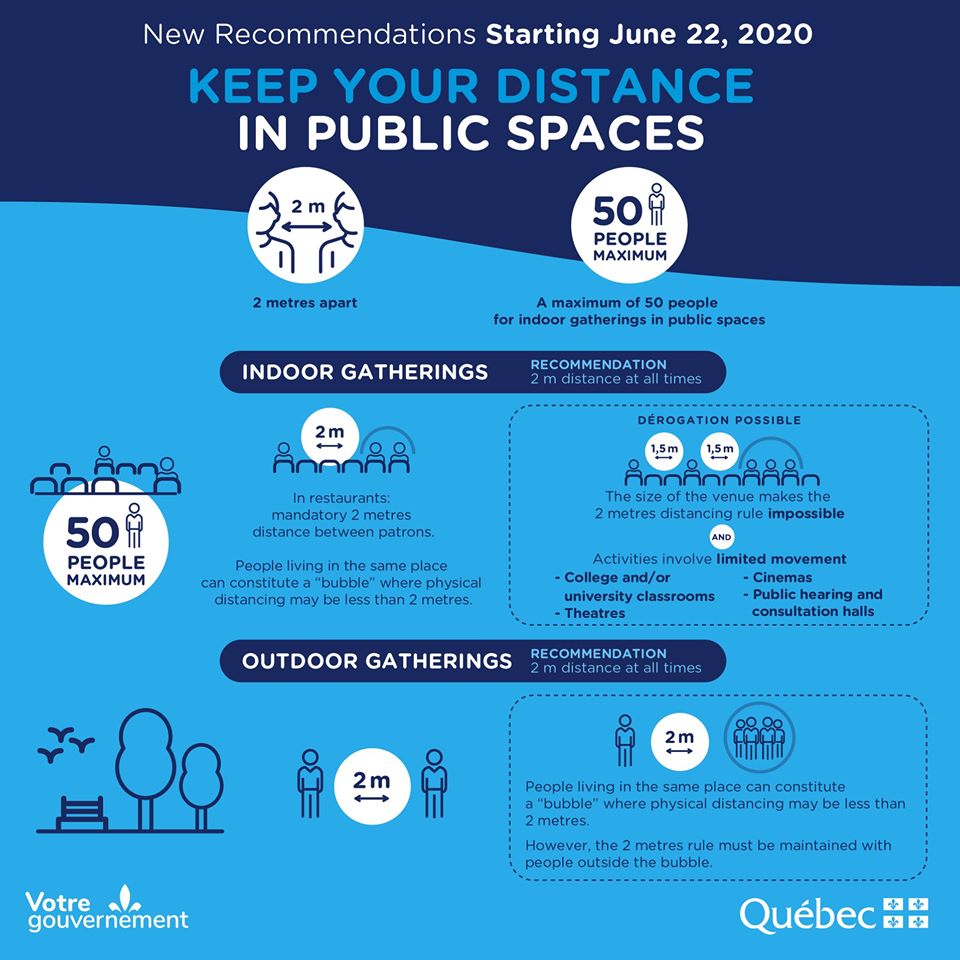
A maximum of 5 households are allowed to meet outdoors, given adequate ventilation and space to allow physical distancing between people from different households. It is important to continue avoiding direct contacts (shaking hands, hugs, etc.), as well as the sharing of food, utensils, etc. Individual sports that can be practiced outside are also allowed (walking, jogging, cycling, etc.). Team sports will resume in Phase 3 only.
- Resuming small scale indoor social gatherings
Indoor social gatherings are now allowed, for a maximum of 2 households, and only those visited already during Goose Break.
- Reopening all local business as well as all local public services
But only if all precautionary measures are in place, including screening for symptomatic workers, self-isolating those who travelled to areas of risk, as well as making sure both workers and clients are observing hygienic and physical distancing measures recommended.
- Resuming all non-essential health care services:
Specialists services, dentistry, or other services, as per local CMC capacity.
- The slow increase of Daycare Centres capacity
Daycare centres will continue to increase their capacity to receive children of parents gradually returning to work. Just like for other local businesses and organizations, centres need to have in place all precautionary measures including screening for symptomatic workers, self-isolating those who travelled to areas of risk, as well as making sure hygienic and physical distancing measures recommended are observed. Each centre should increase the number of children it can accommodate according to its rhythm of adaptation to the measures required; a maximum of 75% of the usual capacity is targeted for Phase 3 only. In addition, day camps will also be allowed to reopen only in Phase 3.
Back to Top
COVID-19 Directive: Restaurant Guidelines - Phase 2
Gradual reopening of restaurants is permitted as part of opening of local business in Phase 2 of Eeyou Istchee deconfinement plan. The following conditions are provided to manage the risk associated with the activity in Cree communities.
I. General preventive guidelines
I.1 Monitoring the risk and health status of workers
- Employers must keep a registry of workers on site every day.
- They must identify workers who may be at high risk of COVID-19. To do so, before allowing a worker on a work site, employers need to ask the following questions:
- Have you been outside the community and in a region considered at high risk in the last 2 weeks?
- Workers answering yes must Self-isolate
- Are you in contact with someone who has COVID-19?
- Workers answering yes must Self-isolate
- Do you have any of the following symptoms: cough, fever, difficulty breathing, sudden loss of sense of taste or smell?
- Workers answering yes must call the local CMC (see Appendix A or https://www.creehealth.org/about-us/contacts)
- Have you been outside the community and in a region considered at high risk in the last 2 weeks?
- Employers must also monitor the state of health of each of their workers on a daily basis, by asking the following question upon arrival at the worksite:
- Do you have any of these symptoms: cough, fever, difficulty breathing, sudden loss of sense of taste or smell?
- Workers answering yes to this question must call the local CMC (see https://www.creehealth.org/about-us/contacts)
- Please note: Temperature taking is not recommended because the results are unreliable, especially for people who work outdoors.
- Do you have any of these symptoms: cough, fever, difficulty breathing, sudden loss of sense of taste or smell?
If there is a case of COVID-19 in the workplace, public health will have to investigate sick worker’s contacts with other people. Depending on the assessment, other workers might also have to be tested and self-isolate for 14 days.
I.2 Promoting physical distancing measures
- Remind all employees to avoid all physical contact (e.g., handshakes, hugs, etc.) poster
- Respect a 2-metre distance between individuals from different households:
- If possible, arrange the work and activity schedule to control the number of persons present at the same time
- Prefer teams that are as small and stable as possible
I.3 Promote hand hygiene and respiratory etiquette
- Providing workers with all necessary supplies (running water, soap, sanitizer solutions, touchless trashcans, disposable tissues, napkins or paper towels, etc.).
- Ensure that hands are washed or that a sanitizer solution is used by everyone, upon entering the organization poster handwashing,
- Encourage everyone to cough into a bent elbow, or into a tissue that is discarded immediately after use, then washing hands as soon as possible poster respiratory etiquette
I.4 Ensure adequate disinfection:
- Disinfect public toilets at least twice per shift, i.e.: once in the middle of the shift and once at the end of the shift.
- Employee Lunchroom cleaning should be done before breaks, before lunchtime, and at the end of the shift.
- Frequently touched surfaces (refrigerators, microwaves, tables, counters, door handles, telephones, computer accessories, sanitizer dispensers, etc.) with the usual cleaning and disinfecting products on each shift.
- .Avoid sharing supplies and equipment (e.g., tablets, pens or pencils, telephones, computers, etc.)
- Remove unnecessary items from common areas (e.g., magazines, etc.).
II. Specific prevention measures – Restaurants
While it is still unclear whether COVID-19 is transmittable through food, respecting good hygienic practices while providing healthy food options are recommended.
II.1. Client reception desk, and the building entrances
- Install disinfecting gel solution dispensers at each entrance (with poster).
- At the reception, Keep a registry of clients who come in.
- Instruct clients to maintain a 2-meter distance between them and the reception clerk
- If not possible, physical barriers (full partitions that are easy to disinfect) should be installed to separate the workers from the customers at checkout, at reception
- Use floor marking to indicate 2 meter physical distance near the checkouts, the reception desk, etc., wherever a line or a bottleneck may form
- Although passing by someone for a few minutes without contact (e.g., on a staircase or in a corridor) does not present a significant risk, it is advisable establish one-way traffic to prevent people from encountering each other, wherever possible
- Limit direct hand-to-hand exchanges of dollar bills, change, credit cards, etc.
- While wearing gloves can prevent contamination when at the cash register, this may give a false sense of security hence increasing the risk of contaminating multiple surfaces due to the gloves not changing them often enough.
- Wearing gloves does not eliminate the necessity to wash hands (hands must be washed every time gloves are removed).
II.2. Employees in contact with food
- Must avoid anyone who shows symptoms of respiratory illness, such as coughing or sneezing.
- The kitchen and service staff must wear a procedure mask and protective eyewear if their tasks make it necessary to be within 2 meters from another person, without a physical barrier.
- If it impossible to wear a procedure mask in the kitchen (too hot and a mask is constantly wet), a visor covering the face from the forehead to the chin can be used
- The constant wearing of protective equipment is preferable than putting it on and removing it repeatedly
- Non-reusable protective equipment should be discarded in containers reserved for this purpose
- A sufficient quantity of personal equipment must be made available to the workers
II.3. Physical arrangement of the table service
- The number of customers in the facility should be limited to allow physical distancing between customers
- if needed, a person at the reception of the facility is responsible for managing the queue
- Limit exchanges of objects with the customers (e.g. present the menus on boards or screens)
- Frequently clean and disinfect the equipment used by all service staff, such as the credit card scanner, cash registers, touchscreens, etc.
- Clients’ used dishes and utensils must be cleaned with dish soap and water, using normal cleaning practices. Using a dishwasher is also suitable.
Sources
https://www.inspq.qc.ca/en/publications/2930-hotel-workers-covid19
https://www.cnesst.gouv.qc.ca/salle-de-presse/covid-19-info-en/Pages/toolkit-restaurant.aspx
Back to Top
Church Services
Many community members have reached out asking when church services can be held again in Eeyou Istchee. Although they cannot yet be conducted in their usual “pre-COVID” fashion, it is certainly possible to plan church services which respect COVID-19 precautionary measures.
Recommendation
Although large indoor gatherings might have to wait until the end of the COVID-19 pandemic, this does mean that church services cannot resume, while still respecting the current limits. Indeed, as long as church services are held in a way which respects physical distancing measures as well as the size limits imposed on the social gathering (limited to 2 households indoors or 5 households outdoor), there is no reason to withhold these activities.
Important caution: Although COVID-19 is not considered to be an airborne disease, some recent research suggests that singing may at times produce aerosols, which could increase the probability of viral transmission. Outdoor services are therefore highly preferable to indoor ones.
The following specific conditions are provided to manage the risk associated with the activity in Cree communities:
1. Monitoring the health risk of community members wishing to attend
Before entering the church service site, whether indoors or outdoors, community members should be asked the following 3 questions:
- Have you been out in a region considered at risk for Eeyou Istchee in the last 2 weeks?
- Have you been in contact with someone who has COVID-19 in the last 2 weeks?
- Do you have any of these symptoms: cough, fever, difficulty breathing, sudden loss of sense of taste or smell?
Note: Temperature taking is not recommended because the results are unreliable; COVID-19 cases do not always present with fever.
- Anyone answering yes to any of these questions must return home and Self-isolate.
- In addition, anyone presenting the above-mentioned symptoms should consult their local CMC, to be examined and tested (see https://www.creehealth.org/about-us/contacts)
- Because of their increased susceptibility to COVID, we also recommend that the following people refrain from attending church services:
- Pregnant women,
- Elders who are 70 years old or older, or
- Anyone suffering from immunodeficiency (cancer patients, for example) or from a chronic disease, which is not well controlled (unstable diabetic, hypertensive or MPOC patients, for example).
- If present, people suffering from these conditions are strongly encouraged to wear a medical mask.
- In addition, organizers must keep a registry of everyone present (whether indoors or outdoors).
- If there is a case of COVID-19 eventually reported in the people attending the service, public health will have to conduct an investigation to determine the level of contact with everyone else present. Depending on the assessment, other people might also have to be tested and self-isolate for 14 days.
2. Promote hand hygiene and respiratory etiquette
- Provide a space, right at the entrance of the outdoor site or of the church itself (for indoor service) where everyone can wash their hands or apply an alcohol-based solution (make sure that it is outside the children’s reach)
- Encourage everyone to cough into a bent elbow, or into a tissue that is discarded immediately after use, then washing hands as soon as possible
- Place posters to remind everyone of the importance of respecting these basic hygienic measures poster hand washing, poster respiratory etiquette
3. Ensure proper physical Distancing
- There is no limit to the number of people present, but sitting capacity must be adjusted depending on the church service site
- If indoors, sitting arrangements should be limited to members of 2 households only
- If outdoors, sitting arrangements (chairs, covers, or else) can accommodate a maximum of 5 households
- Keep a minimum distance of 2 meters (6 feet) between people of different households
- People living at the same address can sit together without physical distancing. (irrespective of how many there are)
- However, it is important to maintain a 2-metre physical distance between people that are not living at the same address (or between the different household groups); it is best to use visual markers to help people know where they can sit.
- Brief interactions (under 15 minutes) that take place between people of different households at less than 2 meters distance is not considered at very high risk and does not require additional measures.
- However, in situations where a longer contact may be necessary (more than 15 minutes) within 2 metres of another person, it is important to wear a mask (or a scarf if no mask is available).
- Everyone is encouraged to wear a mask or artisanal face cover, but these are not an obligation as long as physical distancing is respected; indeed, physical distancing is considered more efficient than wearing masks to protect against COVID-19.
4. Ensure adequate disinfection:
- If the service is held indoors, it is important to ensure proper cleaning and disinfection of the church site (chairs, door handles, toilets if available, etc.)
- It is preferable to avoid serving food or refreshments
Back to Top
COVID-19 Directive: Sports and recreational activities
Some of the sport and recreational activities can be practiced as of Phase 2, to the extent that they comply with the current social gathering restrictions.
For example, as of Phase 2, all sports can be practiced, as long as the following precautionary measures can be respected:
- Outdoor sport activities can be practiced, insofar as all the participants do not represent more than 5 households, and the measures of physical distance between the members of distinct households are respected.
- The practice of indoor activities is limited to participants of 2 households only, also with the restriction of respecting physical distancing between people not living at the same address. Indoors sports are considered at higher risk than those practiced outside, due to the lack of ventilation and space for physical distancing.
While the majority of the guidelines below contribute to mitigating the COVID risk associated with these activities within groups of all ages, the last section presents recommendations that are specific for holding activities with children and youth.
I- Monitoring of high risk workers and participants
- Activity organizers must make sure to identify and exclude all workers and activity participants who are at risk of being infected with COVID-19. To do so, organizers need to ensure the following questions are asked to all workers and participants before they can access the activity site:
- Have you been out in a region considered at risk for Eeyou Istchee in the last 2 weeks?
- Have you been in contact with someone who has COVID-19, or someone who has recently become sick with symptoms that could be COVID-19 in the last 2 weeks?
- Do you have any of the following symptoms, even if they are mild: fever, cough or difficulty breathing, sore throat, fatigue, diarrhea or sudden loss of sense of taste or smell?
- Please note that temperature taking is not required.
- Anyone answering yes to any of the above questions should be excluded from the activity, until they have ended their isolation period.
- In addition, anyone presenting active symptoms must be referred to their local CMC, for investigation and testing (see https://www.creehealth.org/about-us/contacts)
- Finally, organizers must keep a daily registry of everyone present (workers and participants).
- In the event of a case of COVID-19 within the group participating in this activity, public health will conduct an investigation to determine the level of contact with other people. Depending on the assessment, other workers might also have to be tested and self-isolate for 14 days.
II-Promoting hand hygiene and respiratory etiquette
- Provide a space, right at the entrance of the activity site (whether outdoors or indoors), where everyone can wash their hands or apply an alcohol-based solution (making sure that it is outside the children’s reach)
- Encourage everyone to cough into a bent elbow, or into a tissue that is discarded immediately after use, then washing hands as soon as possible
- Place posters to remind everyone of the importance of respecting these basic hygienic measures poster hand washing, poster respiratory etiquette
III-Ensuring proper physical Distancing
- Although there is no limit to the exact number of participants allowed on the activity site, it is important to respect the following activity capacity:
- If the activity is practiced indoors, participants should be limited to members of 2 households only
- If this is an outdoor activity, on the other hand, limit participant number to members of 5 households maximum
- Keep a minimum distance of 2 meters (6 feet) between people of different households
- It is important to maintain a 2 meter physical distance between people that are not living at the same address; however, people living at the same address do not need to physically distance from one another
- This means that there should always be 2 meter distance between groups composed of people living at the same address, but that this is not necessary for people within the group, as long as they all live at the same address., as illustrated below.
- Brief interactions (under 15 minutes) that take place between people of different households at less than 2 meters distance is not considered at very high risk and does not require additional measures.
- For example, passing by someone for a few minutes without contact does not present a risk (e.g., on a staircase or in a corridor).
- However, in situations where a longer contact within 2 meters of a person who is from the same household is necessary, it is important to wear a mask (or a scarf if no mask is available).
- Pay particular attention to areas acting as bottlenecks (e.g., entrance to activity site, changing rooms, etc.): If necessary, position an employee or a volunteer at the entrance to provide instructions and direct participants.
IV- Ensuring adequate disinfection
- If the activity is held indoors, it is important to ensure proper cleaning and disinfection of the activity site (chairs, door handles, toilets, etc.); A frequency of at least once a shift is recommended
- Avoid serving food or refreshments, and ensure each participant have their own snack, water bottle, towel, etc.
- Remove any equipment that is not easily washable and clean equipment frequently, especially those that are manipulated by multiple persons (basketballs, baseball bats, etc.)
V-Measures specific for activities aimed at children and youth
- Because children and youth do not always show clear COVID-19 symptoms, access must be refused not only to children who exhibit symptoms associated with the disease, but also to those who are living with someone exhibiting COVID-19 symptoms, or who is waiting for a COVID-19 test result:
- Any child developing symptoms while on the activity site must be isolated in a room provided for this purpose.
- Only one staff member should be looking after a child exhibiting symptoms while waiting for parents to come to get the child;
- This staff member must wear gloves and an gown, as well as a procedure mask and protective eyewear;
- The parents of the children in the affected group and the staff in contact with the symptomatic child must call the local CMC (see https://www.creehealth.org/about-us/contacts)
- Due to risk of children transmitting COVID-19 to people who are at increased susceptibility of severe COVID-19 infections, we also recommend that children living with household members who present the following vulnerability factors do not attend activities:
- Pregnant women,
- Elders who are 70 years old or older,
- People with a chronic disease or an immunodeficiency, as well as parents whose children suffer from these conditions
- However, these conditions cannot be used to exclude children from activities; the only factor that activity organizers can use to refuse access, apart from its intake capacity, is if a parent and/or child have contracted COVID-19 or have been in contact with a person who has tested positive for COVID-19.
- Modify activities so that they are done outside, as much as possible.
- If held indoors, make sure groups are always assigned the same room.
- Make sure rooms allow a distance of 2 meters to be maintained between persons not living under the same roof
- Form subgroups (of 1 educator with children of similar age group, for example) which remain stable over time.
- Avoid transferring a person from one subgroup to another
Staying Safe During Deconfinement
We would like to remind everyone that we all have a part to play in ensuring deconfinement is safe and successful for our communities:
-
Observe respiratory etiquette (Cough/sneeze in your sleeve. Throw used tissue in a closed garbage can).
-
Avoid touching your face (especially your mouth, nose, or eyes)
-
Thoroughly clean and disinfect public spaces
-
Maintain a physical distance of 2 metres (6 feet) when in public places, particularly among vulnerable
people, including Elders and those with underlying health conditions
-
Stay home if you are sick, or if you have been exposed to the virus
-
Limit non-essential travel. Mandatory 14-day self-isolation after traveling to a high-risk region will continue.
-
Regions considered “high risk” will change as the situation evolves.